Sweet treatment for asthma
A simple molecule inhibits asthma-related inflammation at an early stage
A promising new candidate for an asthma drug has been found: a simple synthetic molecule based on a sugar effectively inhibits the bronchial inflammation that arises with respiratory disease – moreover, at an earlier stage than the current, widely-prescribed asthma drugs. The discovery was made by an international team in which scientists from the Max Planck Institute of Colloids and Interfaces and the Freie Universität Berlin played a key role. As demonstrated by a study on mice, disulphated iduronic acid prevents the development of the processes that result in the secretion of mucus, narrowing of the airways and, ultimately, shortness of breath. Before it can be used in humans, the substance will require further development, and its effectiveness will have to be tested in clinical trials.
Asthma is taking the breath away from increasing numbers of people. In industrialised and emerging countries, the number of patients with the condition has increased steadily for the past 30 years. In Germany alone, three million people suffer from this chronic disease, in which an allergic reaction usually gives rise to the tightening of the chest, shortness of breath and coughing. Inflammatory processes in the bronchia, which involve the constriction of the windpipe and secretion of mucus, play a crucial role here. And this is precisely the targeted area for the substance discovered by an international team headed by scientists from the Max Planck Institute of Colloids and Interfaces in Potsdam, the Freie Universität Berlin and the Sanford-Burnham Medical Research Institute in La Jolla, California.
Sulphated iduronic acid blocks the immune system alarm
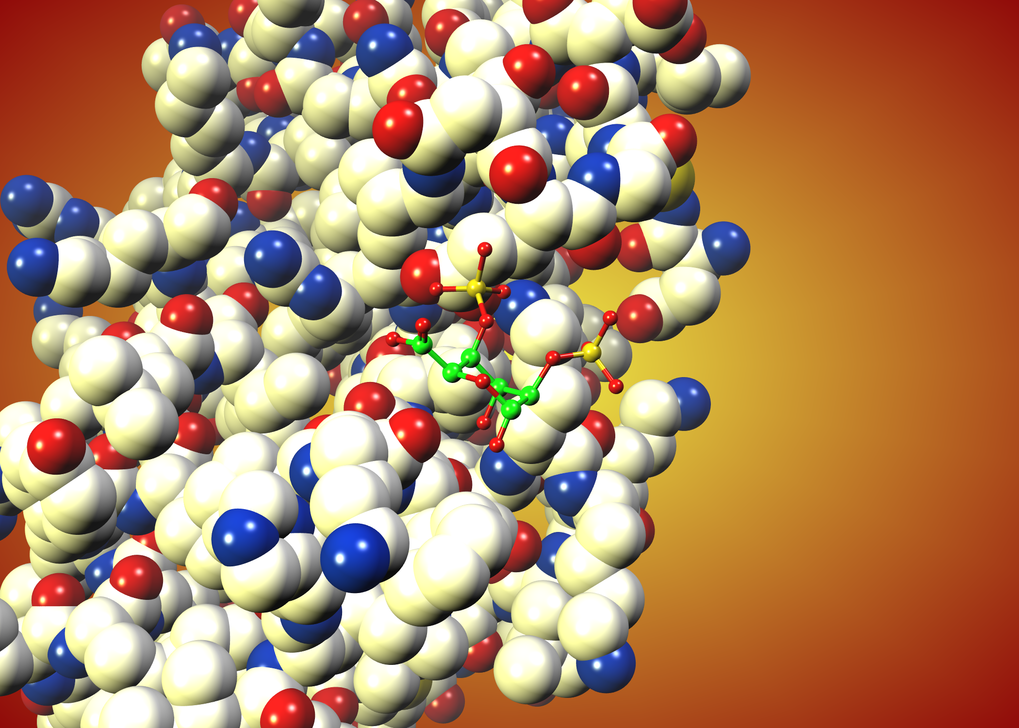
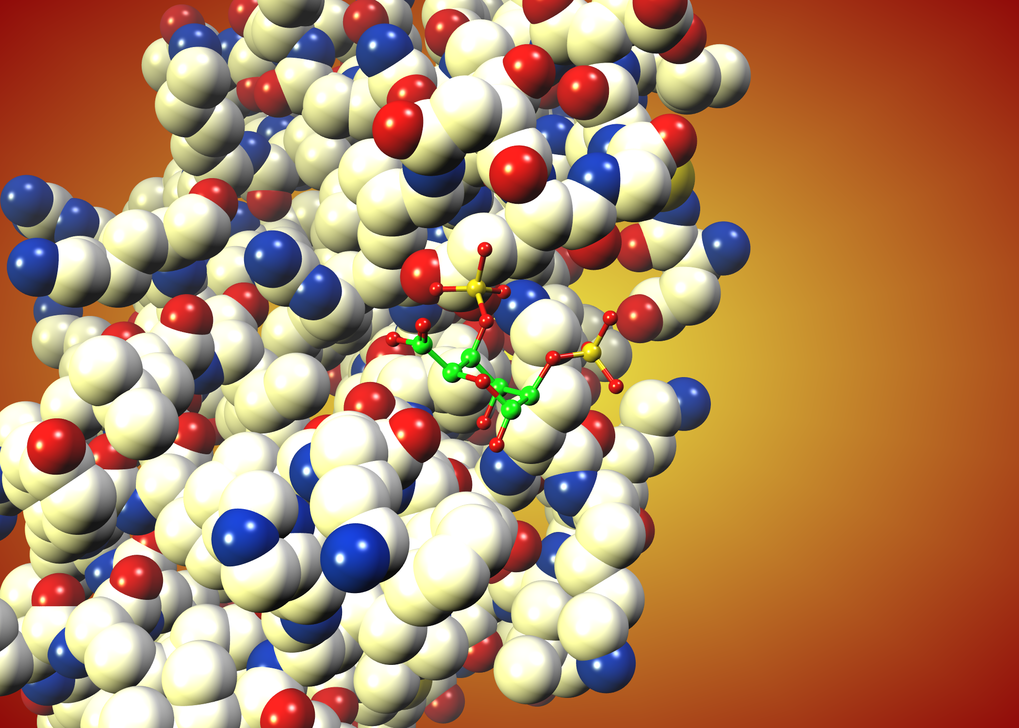
“Our monosaccharide, which is loaded with sulphate groups and does not arise naturally in this form, inhibits the signal that recruits T cells and channels them into the lungs during an asthma attack,” says Peter Seeberger, one of the study’s lead scientists. A Director at the Max Planck Institute in Potsdam and Professor at the Freie Universität Berlin, Peter Seeberger researches the wide-ranging tasks fulfilled by sugars in organisms. In the course of his work, he frequently studies the function of sugars in the immune system, whose protagonists include the T lymphocytes. These cells are a type of white blood corpuscle or leucocyte and play a crucial role in inflammatory processes. During asthma attacks, they are alerted in the course of an over-reaction of the immune system, which occurs when patients come into contact with substances to which they are allergic.
According to the current study, most T leucocytes are alerted during an asthma attack through the docking of the signalling molecule CCL20 at the molecular alarm button CCR6. For the white blood corpuscles to be able to receive the alarm call, however, the CCL20 molecule must team up with a molecule known as heparin or heparan sulphate. Heparin is a chain molecule; its appendages resemble the molecule, with which the international research group has managed to block the immune system’s false alarm. As the researchers established, the sulphated iduronic acid attaches itself to the chemical alarm signal CCL20 instead of heparin, after which the signal is no longer recognised by the CCR6 receiving station.
Effectiveness in humans must be demonstrated in clinical trials
“The fact that – of all things – the simple compound iduronic acid blocks the signalling pathway was a coincidental discovery,” says Peter Seeberger. The researchers initially assumed that this particular molecule was ineffective and initially used it as a control with which to compare the effectiveness of the other candidate molecules. The other test molecules had more obvious similarities with heparan sulphate which, together with CCL20, naturally presses the CCR6 alarm buttons of the white corpuscles: like heparin, these were also chain molecules which are far more difficult to produce than the sulphated iduronic acid.
“Iduronic acid recommends itself as a possible pharmaceutical agent – not least because it is easy to synthesise,” says Peter Seeberger. However, before the sugar derivative can offer relief to patients, it will have to be further developed and go through numerous additional tests. “We will have to alter the substance in such a way that it attaches exclusively to CCL20,” explains Peter Seeberger. Sulphated iduronic acid also attaches itself to other components of the immune system and blocks their activities. This could result in unwanted side-effects; however, the researchers did not observe any such side-effects in the mice. Above all, clinical trials on humans must demonstrate whether the candidate discovered by the team fulfils the promise it showed in the tests on mice. Peter Seeberger has already made contact with medical researchers with a view to confirming this – and met with considerable interest.
PH